MOLD’s series Health. Food. examines narratives around food and healing. Particularly how food feeds into the ongoing maintenance of our bodies, communities, and the Earth.
A recent scientific study quantified the connection between ferments and gut health, finding that people who ate 6 servings of fermented foods a day had increased microbiome diversity and better immune responses. A closer look at the fine print (read: the appendices of the original research article) reveals that six servings in the context of this study meant half a kilogram of sauerkraut/kimchi or a liter of kombucha per day. Aside from the impracticalities of consuming that much salt, acid, and sugar as collateral, the study was heralded as scientific proof that fermented foods are indeed good for you—something nonnas and aunties have known all along—because they improve your microbiome.
The microbiome is a slippery term. In common parlance, it has come to mean all the microbes that live in and on one’s body, representing the individual like a microbial fingerprint. Meanwhile in scientific discussions the term is used with a more medicalized inflection to mean all the genetic material of the microbes that happen to be in that swab, at that time. So the term sometimes refers to the microbes, sometimes genomes; and there is even talk of calling microbiomes a new organ altogether, as if ‘the microbiome’ were ‘the heart’ or ‘the liver.’ Even more slippery is the application of the term ‘microbiome.’ In our current vernacular, someone talking about the microbiome is typically talking about the gut. This is owed in part to the hype surrounding the gut-brain axis in the contemporary moment with exciting research that connects our intestinal health with mental wellbeing. However, many other types of microbiomes — like oral, vaginal or soil — exist all around us. Using the general term ‘microbiome’ to refer to the gut is a sly form of synecdoche, where parts stand as wholes and wholes as parts. Narrowing the term microbiome to the constraints of the gut, as in this case, means that the gut microbiome stands for all microbes that ever were and could be, which grossly overlooks the trillions of other beings that move around and through us at any given time.
This synecdoche of gut-biome-as-whole may seem innocent, but I argue that it conveniently serves the well-worn narrative of eat-this-not-that. My concern is that in the long-term, this approach deprives us of an opportunity to engage with a microbial world upon which our lives depend. To champion ‘the microbiome’ and to ‘eat for it’ changes food ideologies in subtle ways, such that the directive to “eat real food, not too much, mostly plants” (Michael Pollan) or, to “eat whole, unprocessed foods” (Weston Price), seems to have been supplanted with ‘eat ferments, more than you possibly can, and do so for your gut.’
The gut microbiome holds us captive to the promise of mind–body balance: take care of your gut/microbes, and your gut/microbes will take care of you. Baked into this axiomatic language are modern logics of choice and control, with several exhausted metaphors that tangle together.
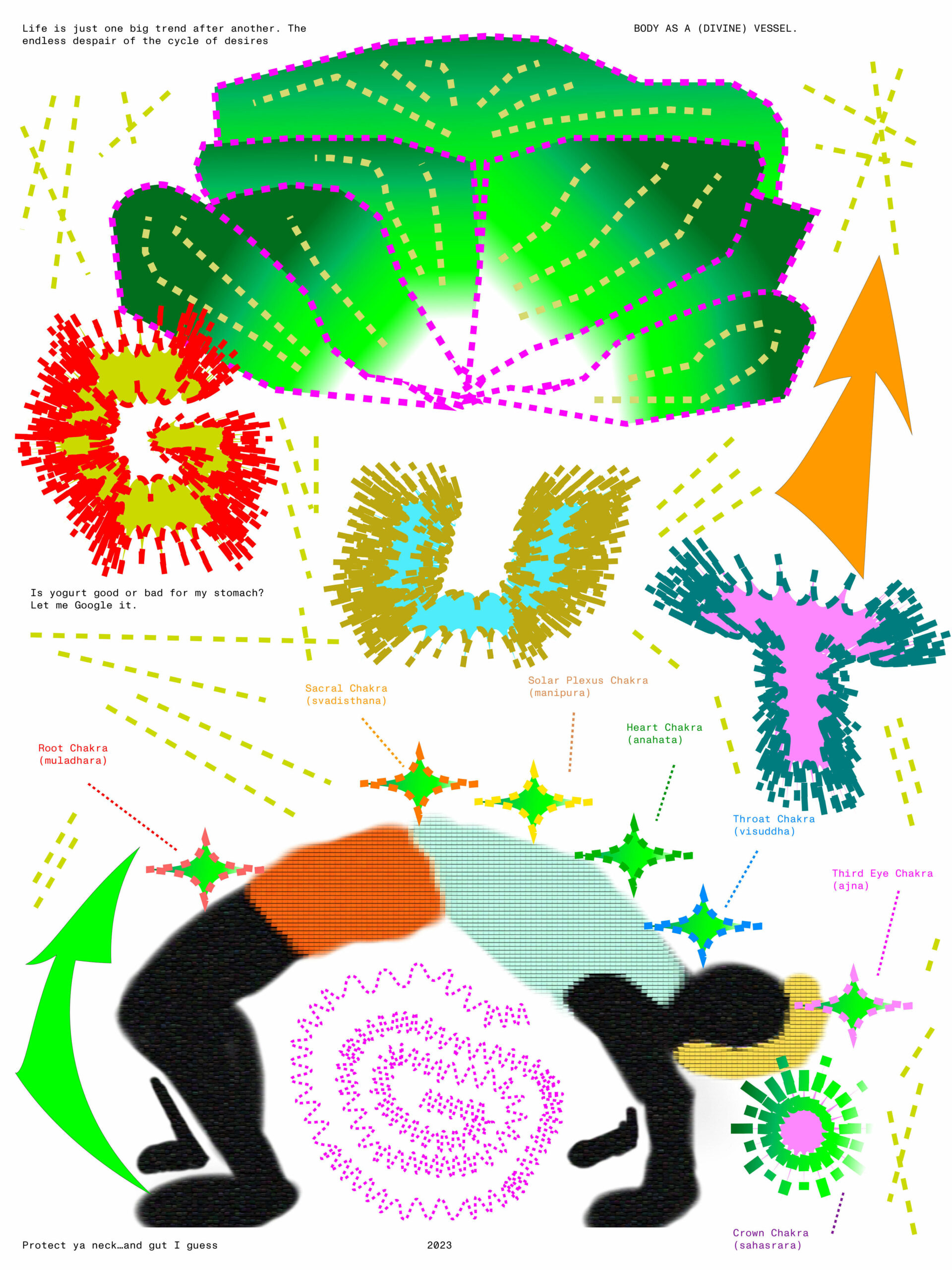
One of the most straightforward metaphors is the idea that the body is a machine, food its fuel, thus coupling inputs like food with outputs like health. The body-as-machine metaphor originated in Cartesian thought and was furthered by the industrializing rhetoric of the 19th century, leading to a reductionist approach to food and health. A mechanistic understanding of the human body was the result, which persists today in how most diets continue to be prescribed and labeled by portions of macromolecules instead of, say, organizing diets around the five tastes or seasonality. “Calories in, calories out” or so the mantra goes, where calorie-control epitomizes the ways that bodies and foods are quantified, standardized, and—considering all of the diet apps and fitness gadgets out there—surveilled. Even the abstraction of kilocalories as something that can be burned like kerosene or butane evokes this fuel-based heuristic. Mechanistic models offer the illusion of simplicity and control, perpetuating a formulaic mindset to food and health. Tabulate the intake, calculate the risk, intervene when the system crashes. Manage your glucose levels! Fuel your body for peak performance! Exercise! Exercise! Exercise! The exhausted metaphor is in itself exhausting.
Many of the verbs used in scientific inquiry around microbes like capture, harness, and exploit, cordons microbes off as just another resource to extract.
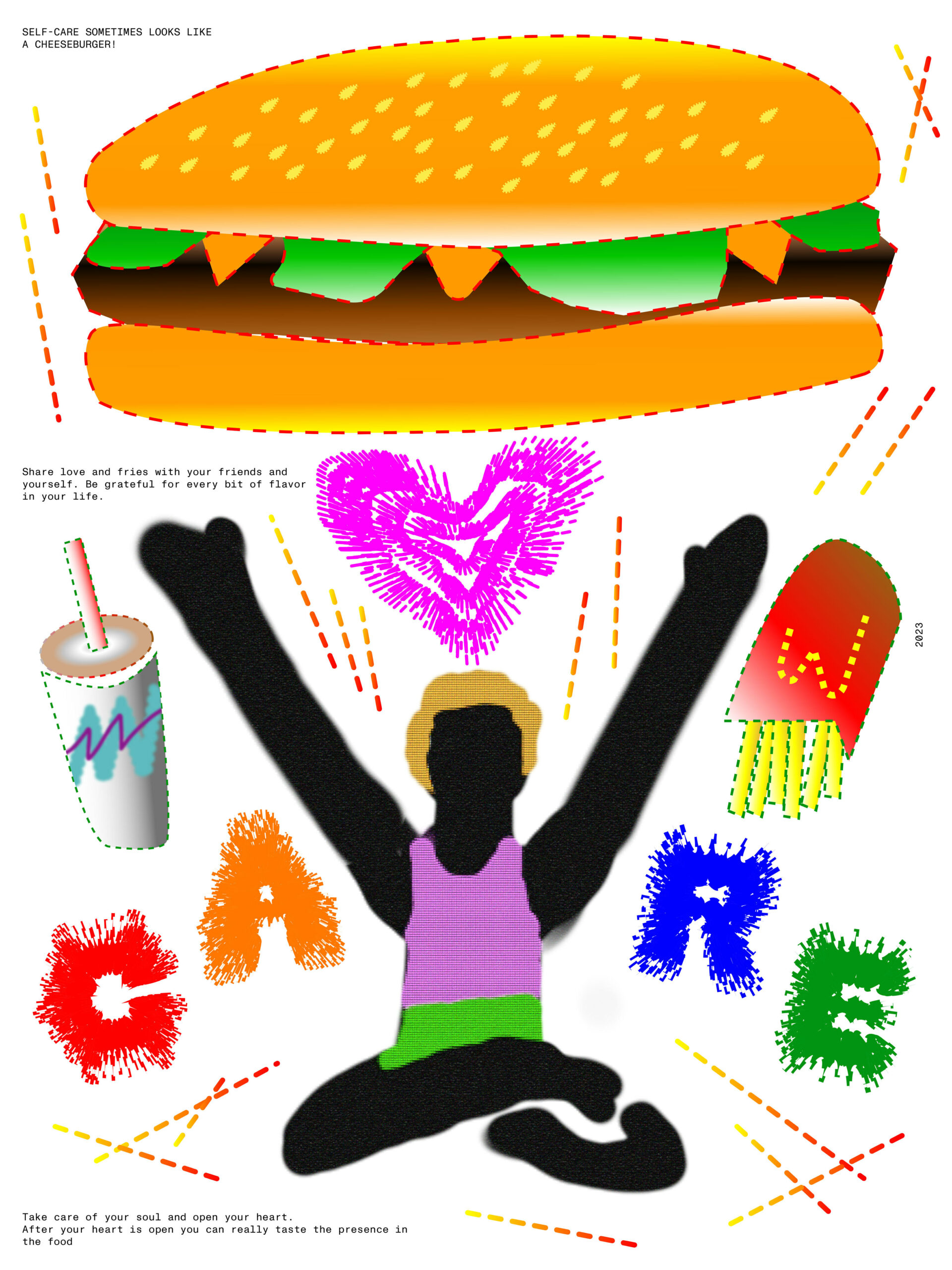
Formulaic and linear approaches to food/health feed into a culture of healthism, an approach to viewing health as a product of individual actions like self-care. Some have noted how “appealing to health allows for a set of moral assumptions to fly stealthily under the radar,” which frames health as a moral project. Healthism conflates the semiotic value of a food with the person eating it. So ‘good’ food makes for ‘good’ personhood, where to eat well is “indicative of self-control and concern for one’s health” while consuming ‘bad’ food signifies “moral weakness.” This reduces health to a series of smart choices about what to eat (e.g., Marion Nestle’s What to Eat), with food know-how and health knowledge serving as signifiers of personal distinction. Social scientist Julie Guthman critiques this insidious attitude, summarizing how these associations between food and personhood reveal (or gloss over) assumptions about race and class with the denigrating lament “if only they knew.” Thus, healthism manifests in the form of moral one-upmanship, where to eat well is to be well and be better than others who share the need to eat but act on it differently.
The human penchant to categorize along the good/bad binary extends to ferments: ‘good’ microbes make up ‘good’ ferments, crystallizing what it means to eat ‘right’ in the current revival of fermentation. It is an enticing thought: to have clarity and consistency across the different microbial characters and know that these are the ones we like, and those ones not so much. Except, microbial identities can shift depending on context. Commensal microbes—which, by definition, neither harm nor help their hosts on their own—can circumstantially become opportunistic if their micro-environments suddenly and temporarily change, sometimes exacerbating diseases, sometimes warding off other infections. In other words, these helpful/harmful identities do not inhere to microbes so much as they are a convenient moniker that we assign to justify utilitarian desires of a human-first capitalism and to obscure the politics of using other critters. Nevertheless, microbial identities become fixed in the product-scape of modern markets. Look no further than the supplement section of a health-food store to see canisters of bacteria like Acidophilus, Bifidobacteria, or proprietary blends of Lactobacilli species. (Chuckle at the fact that a popular yogurt brand made by Dannon Co. attempted to name their flagship bacterial strain Bifidus regularis to evoke and manifest healthy bowel movements, only to be sued for deceptive messaging and misquoting science.) Stool tools maybe, but categorizing microbes along the good/bad binaries always implies how they are good for us and bad to us. All the same, microbes are commonly being mobilized to rectify the so-called imbalances of one’s body. Because at the end of the day, if one fails at the moral project of feeding oneself, there is always a microbe for that.
We can see that many of the ideologies that characterize the state of modern eating responsibilize the individual within the narrow scope of neoliberal agency; and, in the context of ferments and gut health, these ideas enroll certain microbes to be remedial to one’s diet for the benefits they purportedly promise. It is a two-way reductionism: humans are but flawed objects in need of repair and microbes are but shiny tools. Mediating these exchanges, in between, are our gut microbiomes which remain forever-optimizable and elusive—like washboard abs or perfect posture.
I take issue with this framing of microbe-as-medical-supplement for the simple reason that it casts microbes as distinct objects to hunt, name, and consume, instead of seeing them as part of a set of contingent relations that are always (or already) constitutive of our very being. To only see microbes as tools misses the whole point of co-existence. Many of the verbs used in scientific inquiry around microbes like capture, harness, and exploit, cordons microbes off as just another resource to extract. My concern is that championing microbes as tool-first, organism-second means that the modern eater forever stays cradled in the bosom of product-oriented ways of life, instead of cultivating a robust sense of entangled lifeways. It ignores how our collective metabolisms are knotted together, our stakes, entwined.
The latest dietary advice sings to the tune of ‘ditch the probiotic supplements, eat fermented foods instead,’ which reveals the crux of the issue: microbes are alive, whereas shelf-stable products, by definition, are rarely so. At the risk of stating the obvious, live beings need regular feeding, hence the latest emphasis on prebiotics (fiber) to keep microbes alive. Despite this detail, we imagine microbial liveliness in convenient and selective terms: they are alive enough to ‘change’ one’s body from the inside out (in a health sense), but not enough to overtake our system (in a cyborgian sense), hence the auspices of control and the allure of “putting your bacteria to work for you.” Just as well, microbes never quite ‘stay’ with us or ‘become’ us since they mostly pass through our alimentary canals, not unlike tourists in Venice, hence our need to continually seek out microbial foods.
Microbial liveliness comes with three caveats: (1) they need to be fed regularly, (2) replaced regularly, and (3) and we cannot control them anymore than we can will a plant to grow faster. And it is precisely microbial living that enables ours: microbes are crucial to human health because their liveliness entails metabolisms (e.g., short-chain fatty acid production) and metabolites (e.g., vitamin K) that our bodies need. We use microbes and microbial by-products, but unlike animals and animal-by-products, microbes are not alive enough to warrant the same dietary ethics such as vegetarianism or veganism (imagine, if possible, what a diet that does not use microbes would look like). They are a part of our fabric of being.
Microbes are neither singular nor static tools to enact human health. They literally and figuratively thread through us as consortia, animating and animated by our practices with them. Practices as mundane as passing public turnstiles, washing dishes, and petting animals position us in regular contact with microbial life. That is, microbes are not ‘out there’ to ingest; they are always on-the-move, on every surface of every utensil carrying every morsel of every eating encounter; and if they survive the gastric juices of our stomach, they continue on their journey through our intestines, floating along, temporarily setting up residence wherever and whenever opportunity strikes, then live or die according to the food we provide. So yes, in a sense, take care of your gut/microbes! But the reciprocal relation—the clause which assumes that your gut/microbes will, in turn, take care of you—is never a guarantee. This sets up a leery reality where we as humans become dependent on the unpredictabilities of an organism too small, too many, and too difficult to detect. In light of this ontological rearrangement, we are in service of the microbial ‘powerhouses’ that sometimes produce the metabolites we want, but we are neither the manager nor the mechanic of its operations. We are but a mere setting for their temporary colonizing—and only sometimes.
To think of this microbial tapestry as a way-of-life instead of a medical intervention may be the best thing for my mind/body/gut to stay tethered and alive.
Health, then, is less a status to achieve than it is an ongoing negotiation between multiple ecologies woven together. We do not often think of these nested ecologies, how soil ecologies affect kitchen ecologies and everything in between. One tangible example demonstrates this linkage: the microbes that jumpstart the fermentation process for kimchi and sauerkraut come from the microbiome of a cabbage plant, this is in comparison to the microbes of sourdough bread whose bacteria are more likely to come from the bakers’ hands. Thus, the microbes in kraut and kimchi, heralded as ‘healthy ferments,’ are dependent on the microbiomes of the cabbage, the kitchen, the tools, and the techniques that go into making them. In this sense, gut health is not an individual project, and, unless we take care of all other microbial ecologies that shape our food system, gut health will only remain a pipe dream.
Gut-hype is real and rife with assumptions, with undergirding metaphors that are sinister and outdated. Instead of simply focusing on the gut, I propose thinking about health and being—as a thread through us—that acknowledges the various ways we are tethered to one another and our environments. To be sure, we should be weary of only seeing the microbes between us, since it would stoke the fires of biological determinism, genetic chauvinism, and the like. But the relations that microbes make apparent, those are worth paying attention to because they show our interconnectedness. To hail ferments as medicine, then, requires attending to all the ways that the ferment came to be, including the social, cultural, historical, microbial, and the technological forces that transform food to ferment, ferment to a bodily corpus. What I know for certain is that 6 servings of kimchi and kraut do not enable the kinds of relationships I want. They in fact reduce ferments to a delivery mechanism for microbes that I supposedly need, and I have no way of determining if and how those microbes traveled from cabbage to cutting board to fork to alimentary canal in any meaningful way. Rather than eat for my gut/health, I would prefer to see what relations I can cultivate in the long-game of weaving myself into this tapestry of entangled lifeways. To think of this microbial tapestry as a way-of-life instead of a medical intervention may be the best thing for my mind/body/gut to stay tethered and alive.