Shelf Life a monthly series at MOLD that explores how we eat at different stages of life.
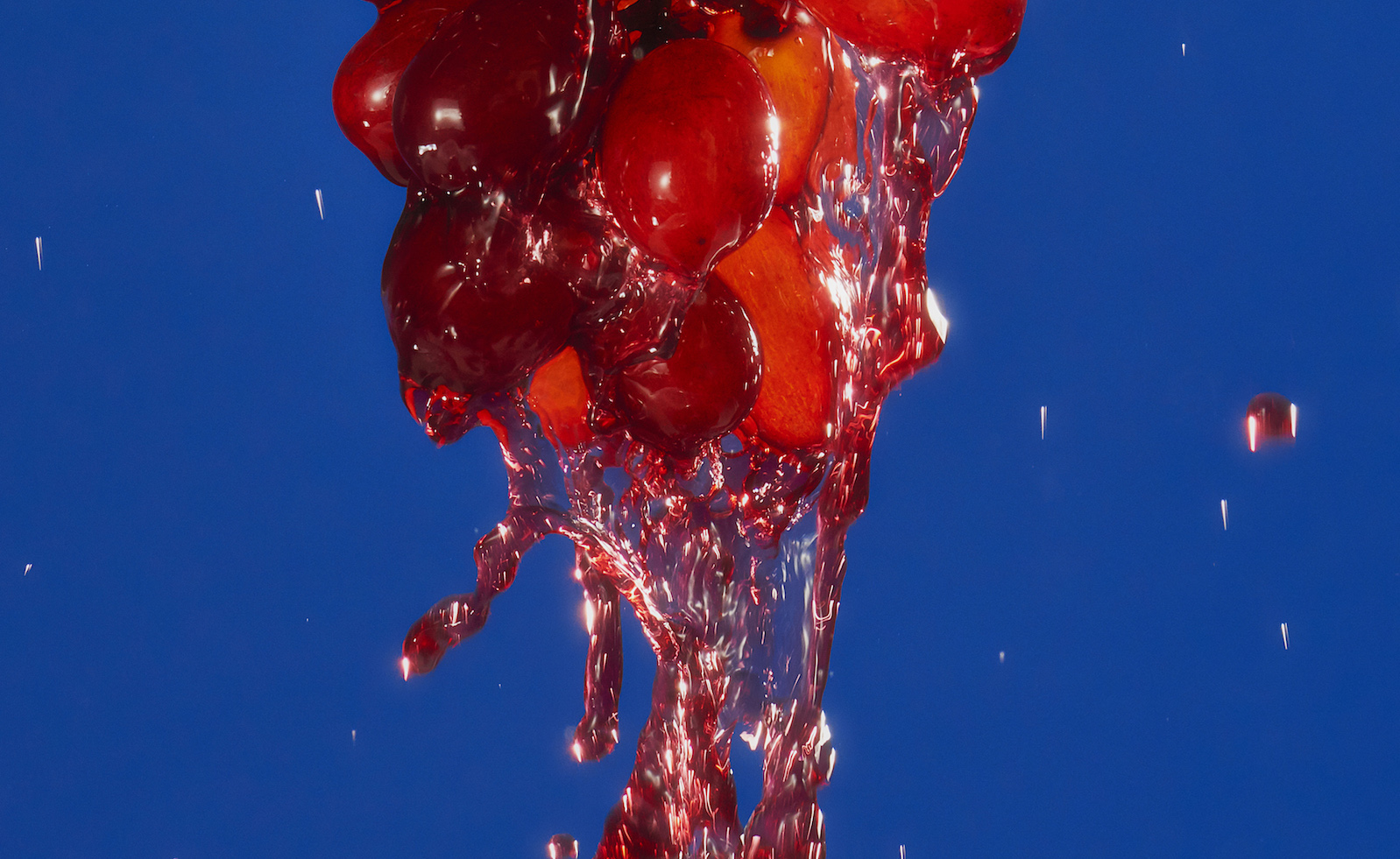
Babies grow very fast from a very small gut. At birth, their entire stomach cavity is rigid and slightly larger than a cherry; over the next thirty days it expands and grows to the size of a walnut, and then to a chicken egg. In our first six months, our stomachs grow over 2,900%, and, for likely the only time in our lives, they do so on a liquid diet.
Newborns need to be fed more fats, protein and other nutrients per ounce than offered in everyday foods. Nature responds by creating breast milk, a hormonal process that extracts nutrients from a mother’s blood supply and transforms them into milk, customized in flavor and viscosity to match a baby’s growth stage and taste palette. Mammary glands regulate production to match demand and adjust milk composition based on health signals in the baby’s saliva. In essence, breast milk is our first and most personalized meal. It may also be our most critical—research has shown that breast milk sets a foundation for our immunological and macrobiotic systems, which are closely intertwined and almost nonexistent at birth. Based on this evidence, scientists at the University of California San Diego are seeking to restatus breast milk as lifesaving tissue rather than food, so that it can be studied as a biotherapeutic agent.
Despite the importance of breast milk, less than half of babies exclusively breastfeed for their first six months, despite what the World Health Organization suggests. It’s one of the few public health challenges where a nation’s wealth has a negative correlation: babies are more likely to breastfeed in developing countries than in the world’s richest nations, says UNICEF. This results, in part, from pressure on mothers to return to work shortly after childbirth and the logistical and social roadblocks for pumping, storing and transporting milk from office to baby. While cultural movements push for dedicated pumping spaces and destigmatized public feeding, product designers are balancing the nuances of infant health, food processing, and workplace realities to create new pump forms (like the Willow, Elvie and Freemie breast pumps that fit into a bra), services (Milk Stork, which stores or ships milk for mothers on business trips), and even content (Virtual Letdown, a VR experience to help mothers relax and pump more efficiently).
But all these product innovations are ineffective in low-technology areas or for families who can’t produce milk. Many of these consumers rely on milk banks, which collect and screen surplus breast milk and freeze it between -20 and -80 degrees Celsius. Yet most milk banks are prohibitively expensive, charging $2-$6 a bottle to offset high pasteurization and preservation costs; even then, milk banks can only store reserves for three months at a time before the milk’s nutritional quality becomes compromised.
In response, scientists are experimenting with ways to make breast milk more shelf-stable. Dr. Blanca Aguilar at the University of Guadalajara has led the effort to adopt spray drying, a technique that sprays each drop of milk to remove moisture but preserve all other characteristics. It’s the same technique used to make flavor coatings for potato chips and prep tomatoes for ketchup; in eight studies between 2016-2019, Aguilar and her team found that spray drying preserves 90% of breast milk’s vital nutrients and is 50 times cheaper than other techniques such as freeze drying. Most importantly, spray dried milk doesn’t need to be frozen or thawed, is lighter to transport, and spills less easily—all qualities that break the threshold for making global breast milk access a public health possibility.
While many work to improve access to breast milk, others are considering its potential to be a vessel for even more nutritional delivery. At Carnegie Mellon University, researcher and new mother Katie Whitehead is modifying cells in breast milk to deliver important medicines to newborns. Spurred by her own experiences breastfeeding, White has proposed that immune cells in breast milk could be engineered to deliver vaccines or stem cells to address birth defects. And in the same way adults are considering their macrobiotic health, scientists at UC Davis are studying changes in microbial diversity for infants who are less likely to be born vaginally (which introduces important bacteria) or might be given antibiotics in the hospital. This research has created a white space for a new class of infant probiotics like Evivo, mixed with breast milk and marketed as baby’s best protection against an unnaturally sanitary world.
No matter how it’s fortified, expelled or processed, breast milk is the only food we naturally produce for our own consumption. It is one of the few meals where we don’t voluntarily control the ingredients and we don’t have to; it is highly designed food at its most primal, recognizing nutritional needs and delivering accordingly. Whether changing the ways we pump or the tools to store reserves, our role is to preserve as much as possible of nature’s work. And there, in breastfeeding, is our first lesson in a lifetime relationship with food.